December 2023. Three years since the height of the COVID-19 pandemic, and it seems that Webbies can finally enjoy a holiday season free of complicated hybrid classes, masking regulations and the general misery brought by the virus.
Though the pandemic may now feel like a relic of the past, the state of public health in the United States and across the globe is far from ideal.
With the rise of seasonal illnesses like the flu and common cold, especially during the winter months, a question arises: how can we prevent ourselves from picking up a disease and experiencing nasty symptoms like coughing, fever and sinus congestion?
Many of these preventative measures are, in fact, common knowledge that our parents recited to us: eat, sleep, stay active, and stay away from germs.
The reality for many students and faculty living on Webb’s campus, however, is that it is near impossible to avoid the coughing, sneezing and cross contamination ever-present in our study and living spaces. This environment, coupled with the post-pandemic uncertainty and constantly evolving Food and Drug Administration (FDA) and Centers for Disease Control and Prevention (CDC) policies, creates a nightmare for communities like Webb, where people of all ages and backgrounds interact daily.
After the return from lockdowns, viruses gained a new chance to attack everyone’s immune systems, which had been weakened from the absence of human interaction. This was especially present at Webb, where students would leave campus in masses to recover in quarantine throughout the 2021-2022 and most of the 2022-2023 school years.
“Sometimes it’s good to challenge your immune system,” said Kimberly Timperlake-Olivares, Certified Pediatric Nurse Practitioner (CPNP). “[Upon return to public spaces] people were hit with all sorts of things: the flu, COVID-19, and RSV (Respiratory Syncytial Virus).”
But when our immune system inevitably fails us this year, where will we go for help?
1. The pharmacy
When it becomes inconvenient to prevent the flu by taking exceptionally precautious measures, we turn to pharmaceuticals — particularly over the counter (OTC) drugs — for relief. Most of us are familiar with Advil and Tylenol, among others, which work against inflammation and general pain. However, there comes a moment for everyone when we realize our cough is persisting longer than we expected, or when the congestion becomes extreme to the point of causing sleepless nights. In this case, people often turn to OTC or prescription drugs for congestion: Sudafed PE, Benadryl, and Dayquil/Nyquil.
The problem with most oral decongestant drugs — those taken in the form of a pill — is the general ineffectiveness that medical professionals have known for decades. This is because by the time the active ingredient in all of these drugs, phenylephrine, passes through the body’s major systems, it is “diluted” until it no longer has a noticeable effect.
“Phenylephrine is something you can get over the counter,” Nurse Timperlake-Olivares said. “A lot of people in pediatrics don’t like to prescribe it because they know it just doesn’t work.”
Although skepticism around phenylephrine has existed since the early 2000s, the FDA only recently confirmed it. In mid-September, an independent Nonprescription Drugs Advisory Committee (a panel of FDA advisors) met and unanimously decided that oral phenylephrine is ineffective in the currently administered dosage.
“With nasal [sprays], it is a different route [of administration],” said Peter Patel, Doctor of Pharmacy, from Hendricks Pharmacy. “It is a quicker delivery system to the affected organs, whether it is the nasal passage or the lungs, as opposed to a PO… which is by mouth. We call it the first pass effect– first, it has to go through your stomach, which has all the acids that degrade [the drug], and it loses its efficacy.”
Many people wonder why phenylephrine-based pills remained the go-to cold and allergy medications for as long as they did, and why it has taken the FDA so long to recognize their ineffectiveness. Surprisingly, the answer traces back to the methamphetamine epidemic of the 1990s and 2000s.
Phenylephrine only really took over pharmacy shelves around 2006, following the passing of the Combat Methamphetamine Act of 2005. This law moved many then-popular OTC decongestant drugs behind the counter in addition to placing harsher restrictions on what and how much people could buy since most of these regulated products were made from either phenylpropanolamine (PPA), associated with increased rates of hemorrhagic stroke, or pseudoephedrine, an essential ingredient in making meth.
The government intended to tackle the issue of rising meth abuse rates through making it more difficult to buy pseudoephedrine, which inadvertently affected millions of people wanting to treat their allergies and stuffy noses.
In addition to phenylephrine gaining a monopoly on allergy drugs following the 2005 law, the process to approve new pharmaceutical drugs or amend existing ones became notoriously long and tedious. Again, the first time that OTC drugs were examined and received high funding by the U.S. government was shockingly recent, with the 2020 CARES Act that provided relief and guidance following the COVID-19 pandemic.
What does all of this mean for those of us who want to buy the right medication to treat our symptoms? The FDA, healthcare professionals, and long-term medication users now all seem to agree that buying any phenylephrine-based drugs is a waste of money, and our efforts are better spent on tried and trusted Advil or nose sprays.
Additionally, Nurse Timperlake-Olivares believes that cough syrup should be avoided when possible.
“We don’t like to give over the counter cough syrups,” she said. “It’s a multibillion dollar industry and people think that you need them, but they can actually make some of the side effects worse… It is very important that if you are going to recommend something as a healthcare provider, that you [make sure] it is actually necessary.
Pseudoephedrine seems to be the only reliable drug for treating congestion, but the existence of many state laws unfortunately means that students under 18 cannot purchase pseudoephedrine, and even those of legal age cannot buy more than nine grams per month. Overall, it is just widely inaccessible to Webb students — so where do we look next?
2. The Health Center
Whenever boarding students (and day students during the academic day) experience symptoms of an illness, or even just general discomfort, we all know that the Health Center is the first place we should turn to — but what does their perspective look like?
“We can recommend things, as long as it’s warranted and it’s safe, that are not necessarily approved for certain ages,” Nurse Timperlake-Olivares said.
Referring to pseudoephedrine-based drugs, Timperlake-Olivares, as a licensed nurse at Webb, spoke about her authority to administer certain medications to students, including minors, when she believes it is necessary. In fact, the FDA often only has age limits on certain medications because they test and approve drugs for those age groups, not because a true danger is posed to younger patients.
She emphasized that with each patient, it is important to assess their situation as a whole — including their history — and not by individual symptoms. Peter Patel agrees, explaining how each student’s immune system has a slightly different tolerance.
“It is individually based — your immune system might be that much better than your peer sitting next to you,” Patel said. “If your greater immunity is stronger, then you might not get the flu and they may.”
As for general treatment and medication, every practitioner can independently decide what works best, taking into account what is safe and accessible for a demographic like the Webb student body. Additionally, diseases can be complex and multilayered, which impacts what the Health Center staff will recommend to students.
“There are fungal infections, bacterial infections, viral infections… they’re all treated very differently,” Nurse Timperlake-Olivares said. “You can have a viral infection, and then get a secondary bacterial infection like an ear infection or a sinus infection. You wouldn’t use an antibiotic to treat a virus, et cetera.”
“I’m a big fan of Tamiflu,” she continued. “It is an antiviral medication we prescribe, and you have to start it really early on. It’s not going to make you not have the flu, but it might lessen the viral load, so you won’t have as strong as symptoms.”
Many other professionals agree that it is just as, if not more, important to take preventative measures to help lessen the load of seasonal afflictions like the flu and cold. There is only so much the Health Center staff and outside nurses can do if we do not take care of our overall well-being, before we become prone to getting sick.
3. Natural Remedies
In the end, many people agree that perhaps the best medicine for winter illness really is time, rest and relaxation.
“A lot of people don’t like to hear that time is ultimately the only thing that will make you feel better,” Nurse Timperlake-Olivares said.
A few things that we can all do before or after we get sick — day students and boarders alike — involve products we probably already have at home or at school.
“If you are super congested, saline flushes, nasal flushes, bulb suctions — especially for children — that’s what’s really going to help you,” Nurse Timperlake-Olivares said. “Humidifiers are wonderful… there’s a lot of supportive [measures] you can take without having to go buy a mainstream medicine that probably doesn’t work.”
“To prevent [illness], you hear it all the time — maintain healthy hygiene, get a flu shot as a preventative measure,” said Patel. “It is not the final answer, but it will lessen the chance of you getting the flu… same with COVID.”
Taking everything into account, we can conclude that students should get preventative vaccines for the flu and COVID if possible and beneficial, and try to keep both their bodies and living spaces as clean as possible. If you truly feel that you need to take medication, first visit the Health Center to get assessed, and then consider getting a prescription medicine instead of a general OTC drug.
If we, the Webb community as a whole, can follow these simple measures, we might be able to enjoy a happy, healthy, 2023 holiday season.





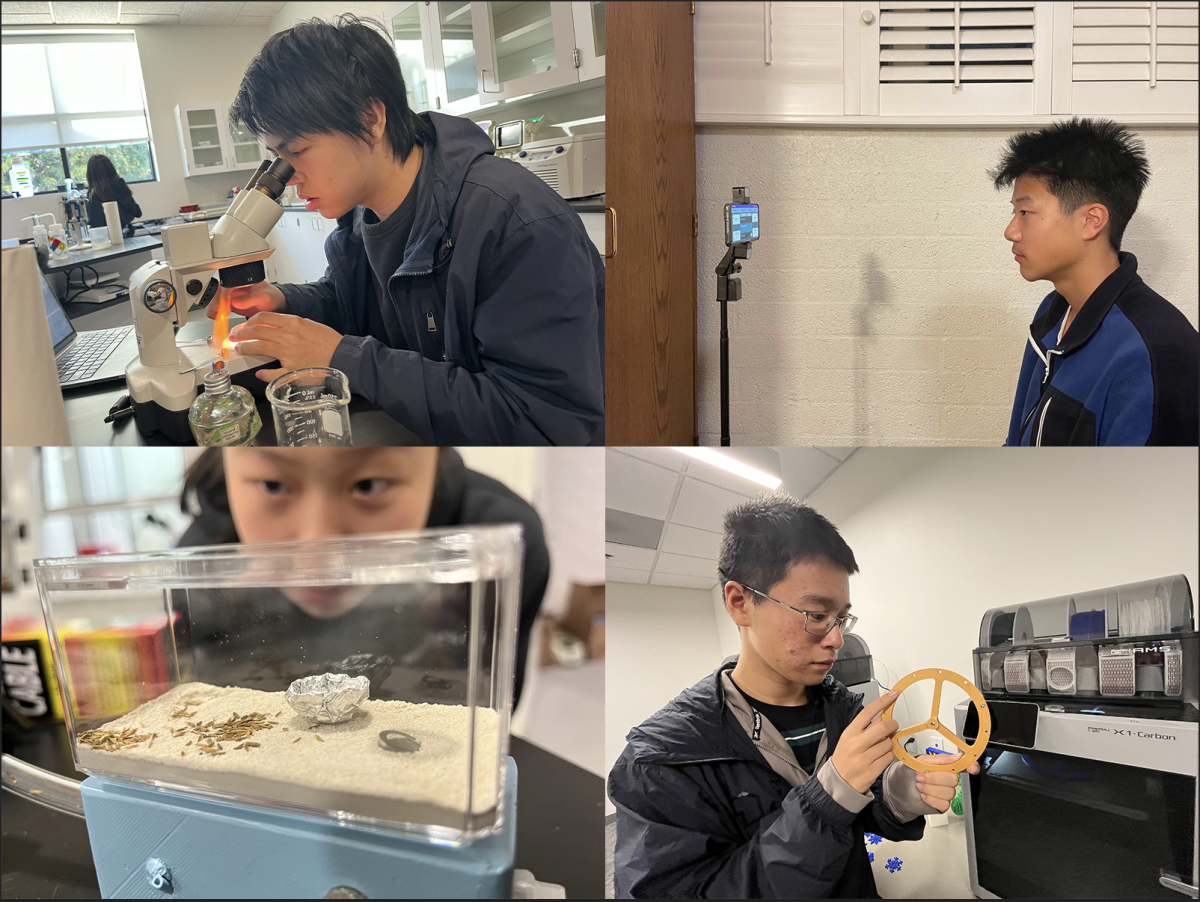
![All members of the Webb Robotics Winter season teams taking a group photo. Of note is Team 359, pictured in the middle row. “It was super exciting to get the win and have the chance to go to regionals [robotics competition]” Max Lan (‘25) said. From left to right: Max Lan (‘25), Jerry Hu (‘26), David Lui (‘25), Jake Hui (’25), Boyang Li (‘25), bottom Jonathan Li (’25), Tyler Liu (‘25)](https://webbcanyonchronicle.com/wp-content/uploads/2025/03/Screenshot-2025-03-10-at-2.41.38 PM.png)